In this ARC Talks webinar, physical therapists Kelsi Schiltz, and Katie Johnson provided recommendations for managing neuropathy symptoms.
Discussion included daily exercises to help mitigate symptoms, what to expect during a physical therapy appointment, and the benefits physical therapy can provide for amyloidosis patients.
Original Presentation Date:
May 23, 2024
Download Katie & Kelsi’s Handout/Guide →
0:00 — Intro
2:31 — Overview
4:56 — What Is Physical Therapy?
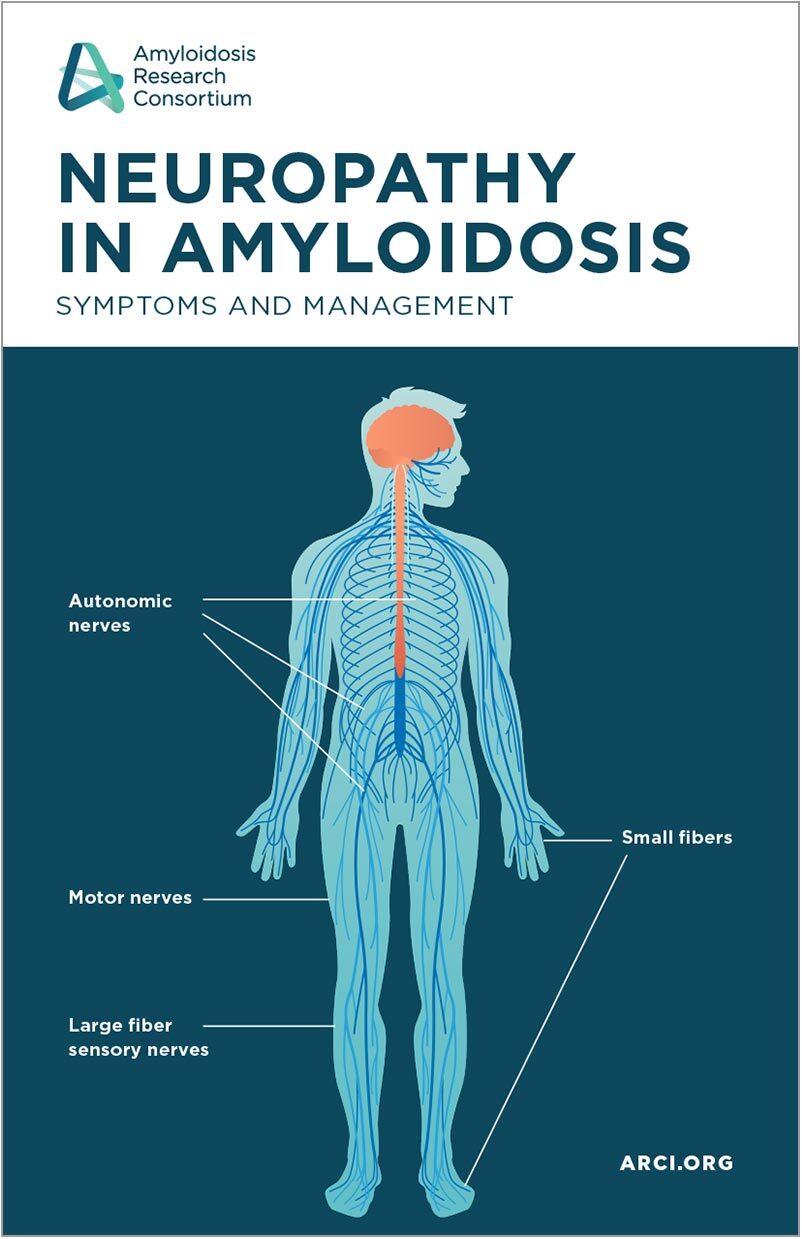
10:23 — What is Neuropathy?
14:12 — How can PT help with Neuropathy?
19:35 — How does Neuropathy impact balance?
24:09 — Neuropathy management & exercises
28:32 — What is Dysautonomia?
34:00 — How can PT help with Dysautonomia?
40:06 — Hydration for Dysautonomia
41:16 — Compression for Dysautonomia
44:13 — Exercises for Dysautonomia
51:39 — Other Therapy for Dysautonomia
53:03 — Q&A Section
53:23 — Can PT help even if I struggle with cardiac involvement?
54:34 — How can I find a PT with amyloidosis experience?
55:52 — Can a PT help evaluate my home so it can work for my needs?
56:41 — Do you have resources for people outside of the US?
57:54 — Can treatment reduce my neuropathy?
Questions Answered After the Webinar:
Q: Do you see double vision issues with amyloidosis? How would/could PT help?
A: Double vision could be a convergence issue with your eyes and this can be addressed in vision therapy with an OT or PT.
Q: Do you recommend core body training to help with fall recovery and strengthening the middle part of the body (e.g. mid-section, arms, shoulders, neck)?
A: Yes, strengthening has been shown to decrease fall risk.
Q: Who can help with accessing in my home a two step stair landing and step down on the opposite side?
A: PTs and OTs (Physical Therapists and Occupational Therapists) can do home evaluations and make recommendations and help train you in your own home.
Q: My main complaint is fatigue. Do you have any tips?
A: Follow the pacing/energy conservation tips provided during the lecture as well as on the handout. It will be important that you start to understand what your limits are/after what activities or interactions you start to notice symptoms of fatigue. The goal would be to stop and rest BEFORE you even notice these symptoms of fatigue. I would highly recommend meeting with a Physical Therapist, Occupational Therapist or Speech Therapist to start working on this—depending on what resources you have around you.
- Start with either taking 5-10 minute rest breaks every hour or complete activities for 20-30 minutes, rest 5-10 minutes, then repeat.
- Sit for activities or household chores—showering, cooking, organizing, getting ready, etc
- Avoid extreme temperatures
- Learn to say no
- Communicate needs or signs of fatigue to family/friends so they can help you stop and rest
Q: Is there a specific PT for carpal tunnel caused by ATTR amyloidosis?
A: Our recommendation would be for nerve flossing/gliding exercises rather than low-load, long-duration stretching (Katie demonstrated this during the lecture in the dysautonomia-mobility section). Meeting with a PT (orthopedic or neurologic) will also help to determine some other specific exercises/nerve gliding exercises.
Q: Sleeping posture: is it best to have the legs elevated?
A: Depending on symptoms and diagnoses. Having your feet elevated can increase the fluid/bloodflow back to your heart and kidneys—this may help with swelling/edema, conversely if you have dysautonomia it WOULD NOT be recommended as this can contribute to dehydration symptoms and frequent nighttime urination/urine production. I would suggest asking your provider to make sure feet elevated is the right answer for you.
Q: I have never had an evaluation more comprehensive than a six minute walk test (6MWT). Where would I go for a more comprehensive evaluation?
A: It sounds like you need a more formal, and specific PT evaluation. Consider your largest concerns—pain, neuropathy, autonomic dysfunction, imbalance/gait, falls, fatigue. These concerns might change which type of PT to recommend. In general, I would suggest finding a Neurologic PT (NCS/Board Certified Clinical Specialist in Neurologic Physical Therapy). They will be most familiar with Amyloidosis and management of this.
- https://www.neuropt.org/consumer-info/what-is-a-neurologic-physical-therapist
- https://www.choosept.com/find-a-pt
- You will have to put in “neurology” in the condition/specialty/diagnosis/name field
- Reach out to Katie or Kelsi and we can help you find one if needed
Contact Our Hosts:
Katie Johnson, PT, DPT, OCS — kathryn.johnson@hsc.utah.edu
Kelsi Schiltz, PT, DPT, NCS — kelsi.schiltz@hsc.utah.edu
Contact ARC:
Call +1 (617) 467-5170
Email ARC at support@arci.org